This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Case Study
Patient N,
Female, Romanian
Table of Contents
Patient Overview
Age at time of treatment: 18 – 25
Injury Level: T7
Treatment Received: Stem Cells, Epidural Stimulation
Location of Treatment: Thailand
Time between injury and treatment: 1 – 2 years
Date of Surgery: 06/04/2018
Date of Discharge: 07/07/2018
Condition on Admission
Patient sustained a complete T7 spinal cord injury in September, 2016, resulting from a car accident. Patient has no motor function and very limited sensory function below the injury level. Patient suffers from neurogenic bladder and bowel, and from significant spasms and spasticity. She does not suffer from neuropathic pain, and is independent in her daily activities.
Previous Therapies & Treatments
Patient underwent spinal decompression surgery on October 13, 2016, and remained in hospital for one month for therapy.
Patient sustained a complete T7 spinal cord injury in September, 2016, resulting from a car accident. Patient has no motor function and very limited sensory function below the injury level. Patient suffers from neurogenic bladder and bowel, and from significant spasms and spasticity. She does not suffer from neuropathic pain, and is independent in her daily activities.
Verita Neuro Treatment Received
After a spinal MRI scan, EMG, and comprehensive blood work, patient underwent laminectomy and implantation of the epidural stimulation device on June 4, 2018. The device is the ‘Medtronic Restore Advance 16-electrode MRI Compatible Device’. The surgery was completed without significant adverse events and no serious complications were reported during the postoperative hospital stay. Surgical wounds healed normally and no spinal cord or superficial wound infection was reported.
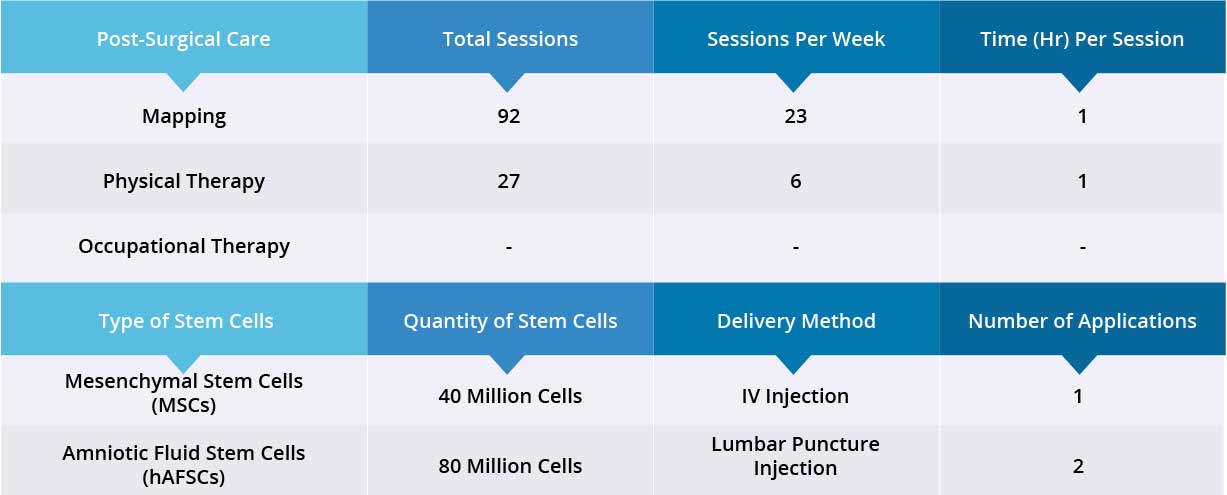
After epidural stimulation surgery, patient received 92 mapping sessions and 27 physical therapy sessions. Patient also received 120 million stem cells: 40 million Mesenchymal Stem Cells (MSCs) and 80 million Amniotic Fluid Stem Cells (hAFSCs) through one IV injection and two lumbar puncture injections, respectively. All three applications went well without adverse effects and no short-term or acute complications have been reported.
Device mapping and therapy were carried out after surgery for 35 days, then patient was discharged.
Results
- Motor Functions
- Sensory Functions
- Autonomic Functions
Patient has good static sitting balance with minimal support required, but dynamic sitting balance is not possible yet. Patient required two people to assist in standing, but has good static standing balance with minimal support and is able to stand at the parallel bar and lock both knees and hips. Patient has good trunk control and bears weight equally on both legs while standing. Patient did not require a hoist while standing or during stepping exercises. Patient experiences significant spasticity, so she had slight difficulties taking unassisted steps but is able to take assisted steps. Patient did require assistance locking knees and hips when stepping and was able to lift her feet, but required assistance in foot placement. Patient is not able to coordinate both legs during stepping exercises.
There was no noticeable improvement to her neurogenic bladder and bowel. Patient received stem cell injections, therefore we expect to see results in these areas within 3 months. After 35 days, patient was discharged and will continue her physiotherapy back home
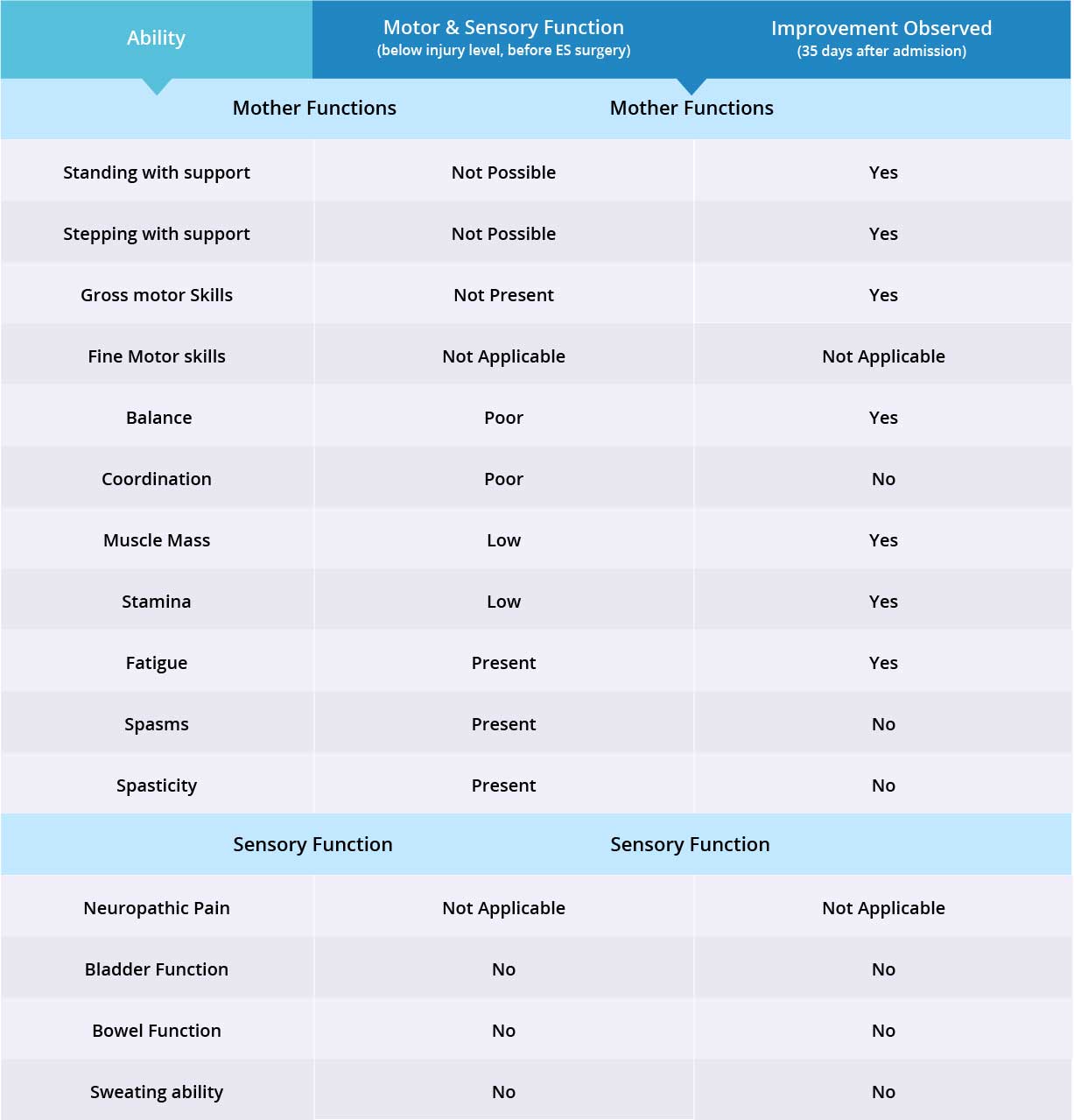
Improvements are monitored in 15 targeted areas: 11 Motor areas and 4 Sensory areas. However, the number of targeted areas may vary depending on patient’s condition prior to admission. If patient does not experience symptoms in certain Motor/Sensory functions, or is not impaired in a specific targeted area prior to surgery, it is excluded from the report (Not Applicable). If there is progress in any given area — either mild, moderate, or significant — it is measured and reported as positive (“Yes”). No improvement, the existence of pain or spasms, or an inability to perform a measured function is reported as “No”.
Results Interpretation
Patient is paraplegic with normal upper limb function, therefore 10 of 11 motor function areas were measured. Motor function improved in 7 out of 10 targeted areas when the epidural stimulation device was switched on.
Patient does not suffer from neuropathic pain, therefore 3 of 4 sensory function areas were measured. Patient has not experienced any changes in the three measured sensory function areas, but more feedback will be collected after 3 months to note any improvements made by regenerative medicine treatment. Overall, improvements were recorded in 7 out of 13 targeted motor and sensory function areas.